
September 3, 2024
Menopause And Urinary System Incontinence

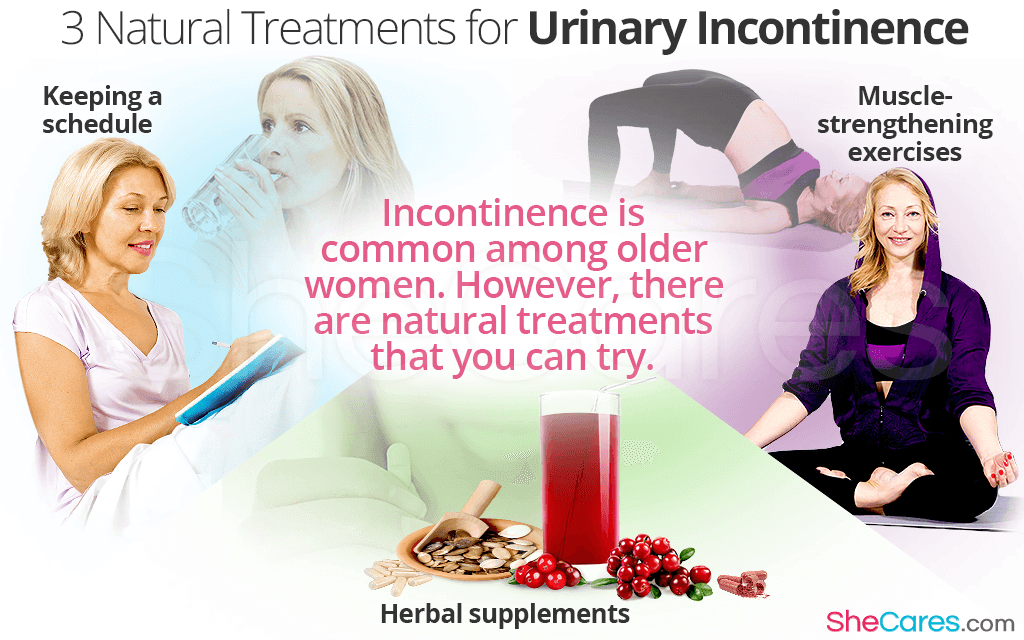
Treatment
What foods stop urination?
- Typically, the quantity of ADH in the body is higher during the evening. This helps avoid peeing while you are sleeping.
- But if the degrees of ADH stay reduced throughout the night, the body will create big amounts
- of pee, so urination
- during the night is most likely
- .
- Hormone control or birth
- control medication.Hormone replacement medications.Anti-androgen medications.Vaginal estrogen.Clomiphene and letrozole.Assisted reproductive technology.Metformin.Levothyroxine. The pee quantity law is maintaining the electrolyte in balance. The hormonal agents that are accountable for urine quantity are Aldosterone, Antidiuretic hormone and Atrial natriuretic peptide. The hormonal agent estrogen plays a major function in females. It is mostly in charge of a woman's regular monthly period, developing the thick cellular lining of the womb and releasing it throughout the menses. It additionally helps the pelvic floor to be solid and supple, giving higher control over bladder and digestive tract features.
Factors To Choose Laparoscopy Over Traditional Therapy
Figure out if you certify to get urinary incontinence products cost-free through your insurance policy at the bottom of the web page. An individual should speak to a physician if they have any worries they may have low estrogen or if they are experiencing bladder signs. Reduced estrogen can also impact people beyond menopause, especially after delivering or during breastfeeding. As numerous as 15% of premenopausal females may have GSM-like symptoms consequently. Nonetheless, they can also go down during other phases of life, such as after delivering or while breastfeeding. Throughout this procedure, the posterior wall of the urethra shears off the anterior urethral wall surface to open up the bladder neck when innate sphincter deficiency exists. Functional urinary incontinence is the lack of ability to hold urine because of factors besides neuro-urologic and reduced urinary system disorder. Videourodynamic studies are booked to review complex cases of anxiety urinary incontinence. Urethral inexperience generally results in recurring urinary system incontinence, usually at rest. Hormonal agent therapy (estrogen) in postmenopausal females alleviates urinary regularity which leads to increase in the toughness of muscular tissues around the bladder. Althoughbasic science in this field is limited, a recent placebo-controlled, randomizedclinical trial of estrogen alone sheds light on this issue. Urethral closureis depending on the integrated action of the Bladder Training suburethral genital wall surface, thepubourethral ligaments, the pubococcygeus muscles, and the paraurethral connectivetissues. As you age, the muscle mass that support your pelvic body organs can compromise. This suggests that your bladder and urethra have much less assistance-- frequently resulting in pee leakage. This indicates that those components of your body change as the degrees of estrogen adjustment. The study consisted of 133 pre-menopausal ladies with routine durations that were not taking hormones. Out of the 133 females, 41% reported experiencing urinary incontinence at different times throughout their periods. Well, while there isn't much urodynamic research study to explain the partnership between menstrual cycles and urinary incontinence, there is a prevalence of urinary incontinence signs throughout women's periods. Both menopause and recent giving birth associate with a higher threat of other concerns that may create bladder problems, such as pelvic floor injuries.- If you have a chronic problem like diabetes mellitus or multiple sclerosis, you might have incontinence for a. long period of time.
- The suggested dose is 1.5 to 2.0 mg/kg twice daily to three times daily.
- In some cases it is the initial and only sign of an urinary system system infection.
Social Links