September 13, 2024
Urinary System Incontinence: Medlineplus Clinical Encyclopedia
Treatment Of Mixed Urinary Incontinence Pmc As the term suggests, combined urinary system incontinence implies that a woman complains of both anxiety and advise incontinence-- spontaneous loss of pee with necessity and with physical exertion, sneezing or coughing. Blended incontinence may be prompt predominant, stress and anxiety predominant, or equivalent. The pathophysiology and treatment of blended incontinence have actually not been well studied although that it represents one-third of incontinence complaints. Pelvic floor muscular tissue exercises and behavioral training are proper first-line therapies for both sorts of urinary incontinence (see the stress and urge incontinence areas presented earlier). Psychophysiological feedback provides a certain reinforcement for pelvic contraction that is separated from the disadvantageous abdominal tightening. For that reason, understanding of levator rectum contraction can be accomplished more efficiently making use of biofeedback than vaginal palpation alone. People that benefit most have a tendency to be young healthy and balanced women who can identify the levator rectum muscular tissues (specifically, the pubococcygeus part) precisely. Older adults with weak pelvic muscle tone or women who have problem identifying the proper muscular tissues need adjunctive treatment such as psychophysiological feedback or electric excitement. For lots of people, straightforward way of living and dietary changes or treatment can treat symptoms of urinary system incontinence. In addition, urinary incontinence is underdiagnosed and underreported. An estimated 50-70% of females with urinary incontinence stop working to look for medical assessment and treatment due to social stigma. Only 5% of incontinent individuals in the community and 2% in nursing homes receive ideal medical assessment and therapy. Individuals with urinary incontinence frequently deal with this condition for 6-9 years prior to seeking medical treatment. In combined urinary incontinence, the bladder electrical outlet is weak and the detrusor is overactive.Am I At A Higher Risk Of Incontinence At An Older Age?
Client acceptance can be reduced because of the discomfort of wearing the probe for a number of hours each day. Consequently, advising the individual in the checking out area by having her capture the examiner's intravaginal or intrarectal finger is important. Potential risks consist of cystitis, pyelonephritis, urosepsis, and bladder perforation. Hence, Foley catheter securing is not generally employed except in those uncommon events where bladder restoration is being pondered. The clamping ought to be done under strict guidance, with monitoring of patient comfort and bladder capability.Therapies And Therapies
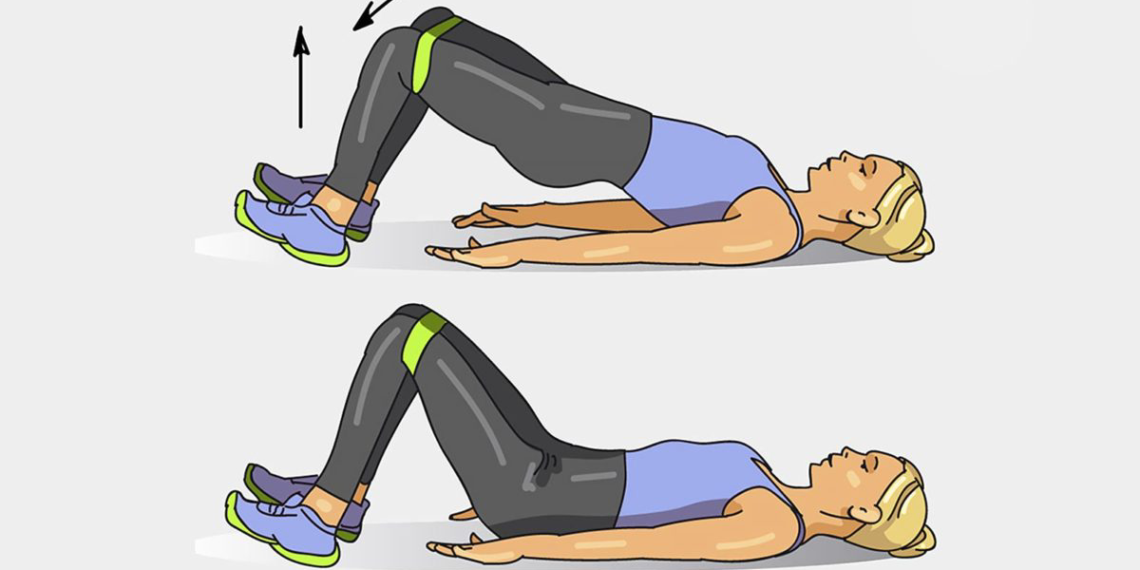
Vaginal cones may be utilized to assist with pelvic flooring muscle training. If you can get your pelvic floor muscular tissues, you'll be offered a workout programme based on your analysis. The professional will assess whether you have the ability to capture (contract) your pelvic flooring muscle mass and by how much. A GP may refer you to an expert to begin a program of pelvic floor muscle mass training. This will depend upon the reason and kind of incontinence you are experiencing. Caffeine is a natural diuretic and has a direct excitatory impact on bladder smooth muscle. Hence, caffeine-containing items produce excessive urine and worsen signs of urinary regularity Surgery and urgency. Some examples of hot spices include curry, chili pepper, chili pepper, and dry mustard. A couple of clinical records have actually indicated that the evasion of spicy foods might have an advantageous effect on urinary system incontinence. These connective-tissue components form the passive supports to the urethra and bladder neck. Throughout times of enhanced intra-abdominal stress, if these supports are undamaged, they enhance the encouraging impact of muscular closure of the pelvic floor. There are many different factors that your doctor will consider when producing a therapy plan for your incontinence. The sort of incontinence and the ways it impacts your life are both big factors to consider. Your provider will certainly likewise speak to you about the sort of treatment you are most comfortable with.- Professional trials (eg, with indomethacin) have actually shown blended and typically not impressive results.
- By jotting down how commonly you experience incontinence problems over the span of a couple of days, your service provider may be able to identify a pattern.
- Individuals with urinary incontinence often cope with this problem for 6-9 years prior to seeking medical treatment.
- Coadministration with CYP-2D6 substrates that have a narrow healing index (eg, flecainide, thioridazine, TCAs) may trigger toxicity of these various other 2D6 substrates.
What is the best treatment for urinary system incontinence?
Liquid and diet plan monitoring, to gain back control of your bladder. You may need to reduce on or prevent alcohol, caffeine or acidic foods. Reducing liquid consumption, reducing weight or boosting physical activity additionally can ease the issue.
Social Links