September 6, 2024
Pee Urinary Incontinence An Overview
Stress And Anxiety Incontinence: Reasons, Symptoms And Therapy [23] is labelled the relationship between menopause and urinary incontinence that women with urinary system incontinence than those that did not have, significantly had greater BMI [24] Healthcare specialists ought to think about urinary incontinence a scientific priority and develop suitable analysis skills. They must have the ability to identify and handle any type of pertinent modifiable factors that might relieve the problem.Therapies That Trigger Hormone Signs
What is the most effective therapy for bladder leak?
Information From Mayo Clinic
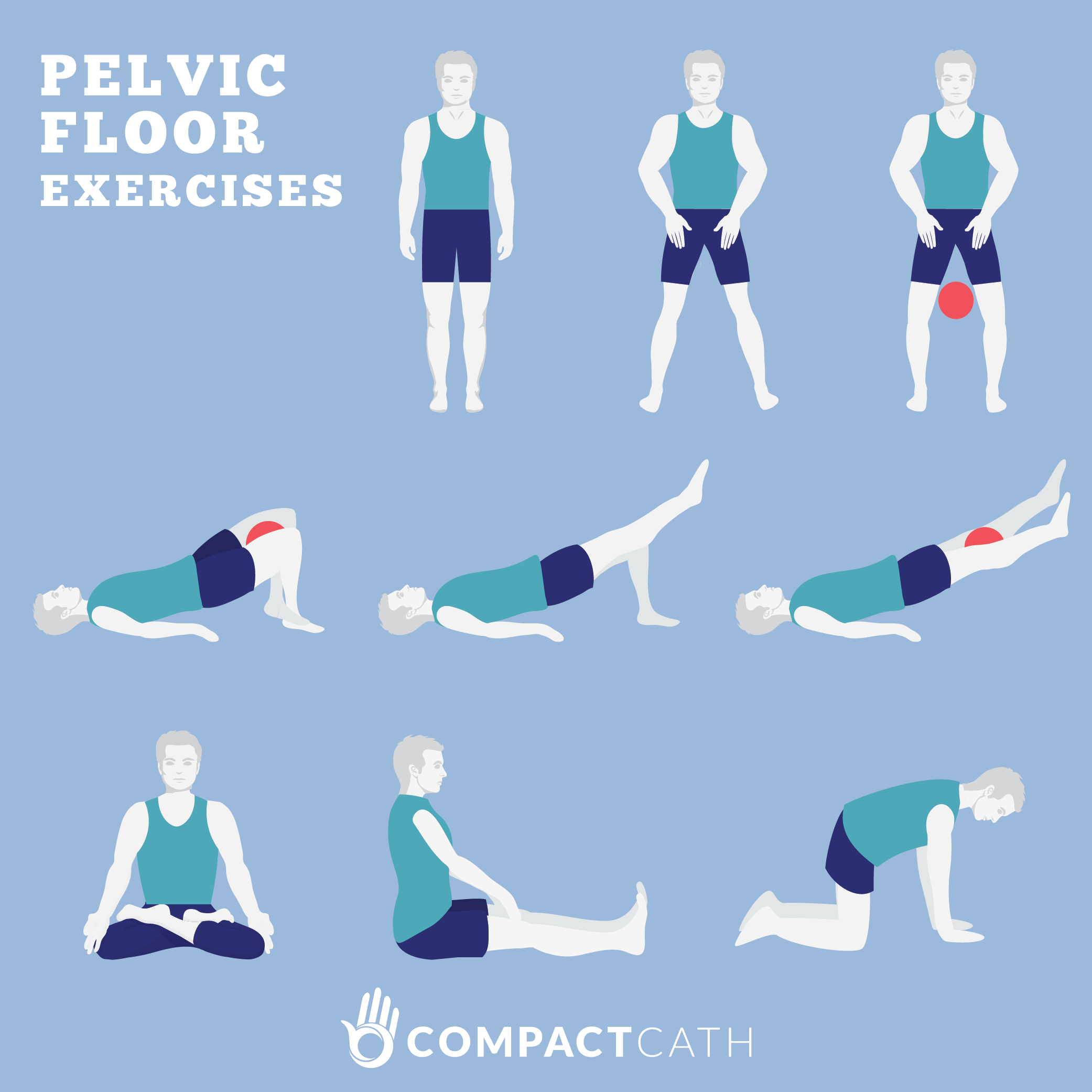
Throughout a woman's life, from adolescence to menopause, the delicate balance of hormonal agents orchestrates a harmony of adjustments that can affect urinary continence and pelvic floor stamina. Often, there are changes to your daily life that can in fact assist your incontinence. These adjustments usually consist of exercises you can do to reinforce your pelvic flooring muscle mass, modifications to your typical habits and an improved diet regimen. Some people notice improvements by making these adjustments in your home and do not need additional treatment. These hormone changes can affect bladder feature and urinary routines, materializing as urinary system symptoms such as increased frequency, urgency, or leakage. Low degrees of estrogen and urinary incontinence go hand in hand. As females age and start coming close to menopause, the ovaries slow down the process of making estrogen, and the levels of this women sex hormonal agent naturally decline in the body. [newline] At some point, with menopause, the production of estrogen stops, and this affects the body in lots of methods. Without estrogen, females discover it difficult to preserve healthy and balanced urologic features during and after menopause. Bladder control for ladies begins along with their final menstruation duration and boosts after that. Urethral incompetence usually results in recurring urinary incontinence, usually at rest. Hormone therapy (estrogen) in postmenopausal women minimizes urinary frequency which causes boost in the strength of muscular tissues around the bladder. Althoughbasic scientific research around is restricted, a current placebo-controlled, randomizedclinical test of estrogen alone sheds light on this issue. Urethral closureis dependent on the integrated activity of the suburethral vaginal wall, thepubourethral ligaments, the pubococcygeus muscles, and the paraurethral connectivetissues. As you age, the muscles that sustain your pelvic body organs can deteriorate. This indicates that your bladder and urethra have much less support-- frequently leading to pee leakage. This indicates that those components of your body change as the levels of estrogen change. The research included 133 pre-menopausal females with regular durations that were not taking hormones. Out of the 133 females, 41% reported experiencing incontinence at different times during their periods. Well, while there isn't much urodynamic research to explain the partnership in between menstrual cycles and urinary incontinence, there is a frequency of incontinence symptoms throughout women's periods. Both menopause and recent giving birth associate with a higher danger of other problems that may create bladder issues, such as pelvic floor injuries.- A physiotherapist that concentrates on pelvic flooring conditions can assist you understand the correct strategies.
- The tool suits the vaginal canal and offers assistance to vaginal cells displaced by pelvic body organ prolapse.
- Without estrogen, ladies find it hard to keep healthy urologic features throughout and after menopause.
- Urinary incontinence is specified as the unchecked loss of urine, usually in an unfavorable location, developing social and hygienic troubles.
Regarding Mayo Facility
They'll initially intend to try the things that have the least influence on your body. Information given on https://5ghb9bmaj7etny.s3.us-east.cloud-object-storage.appdomain.cloud/Pelvic-floor/vaginal-firmness/tension-urinary-incontinence-truth-sheets-yale.html the Aeroflow Urology blog site is not intended as a substitute for medical advice or care from a health care specialist. Aeroflow suggests consulting your healthcare provider if you are experiencing medical concerns connecting to incontinence. Additionally referred to as Kegel exercises, these workouts can assist improve the stamina of your pelvic flooring. Even if you don't have incontinence, you should do pelvic flooring workouts to assist keep your pelvic area strong and continent. The fluctuation of progesterone and estrogen is why you experience symptoms throughout your cycle and while on your duration.Social Links